![Cell recycling (shown in green) is elevated in lung cancer cells treated with an established cancer drug. Recycling is suppressed upon co-treatment with a newly discovered enzyme inhibitor. [Salk Institute]](https://genengnews.com/wp-content/uploads/2018/08/June26_2015_SalkInst_CancerCellRecyclingShutdown1194046252-1.jpg)
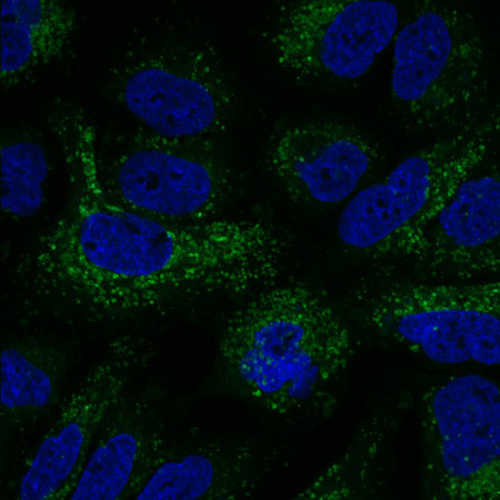
Cell recycling (shown in green) is elevated in lung cancer cells treated with an established cancer drug. Recycling is suppressed upon co-treatment with a newly discovered enzyme inhibitor. [Salk Institute]
Unlike many last stands in human history, the last stands arranged by individual cancer cells often resist being overwhelmed, with dire consequences for cancer patients. Cancer cells maintain themselves by co-opting autophagy, an energy-harvesting process that is normally used to recycle damaged organelles and proteins. Autophagy is especially important to cancer cells that have been cut off from nutrient pathways, due to the attacks of cancer drugs such as rampamycin (mTOR) inhibitors.
Now it appears a coordinated attack may be possible, one that would not only disrupt nutrient uptake, but also prevent nutrient recycling. In such an attack, the task of shutting down recycling could be assigned to a new autophagy-inhibiting drug. This drug, which is called SBI-0206965, could make it possible to overrun cancer before it musters one last defense, and gives itself a chance to fight another day.
The new drug targets ULK1, an enzyme that initiates autophagy. The drug, which was developed by scientists at Salk Institute and Sanford Burnham Prebys Medical Discovery Institute (SBP), was described June 25 in Molecular Cell, in an article entitled, “Small Molecule Inhibition of the Autophagy Kinase ULK1 and Identification of ULK1 Substrates.”
“[We] screened degenerate peptide libraries to deduce the optimal ULK1 substrate motif and discovered 15 phosphorylation sites in core autophagy proteins that were verified as in vivo ULK1 targets,” wrote the authors. “We utilized these ULK1 substrates to perform a cell-based screen to identify and characterize a potent ULK1 small molecule inhibitor.”
According to this study, SBI-0206965 proved to be a highly selective ULK1 kinase inhibitor in vitro, and it suppresses ULK1-mediated phosphorylation events in cells, regulating autophagy and cell survival. In addition, SBI-0206965 combined with starvation or mTOR inhibition leads to ULK1 degradation. Essentially, SBI-0206965 synergizes with mTOR inhibition to induce cell death.
“The finding opens the door to a new way to attack cancer,” said Reuben J. Shaw, Ph.D., a senior author of the paper, professor in the Molecular and Cell Biology Laboratory at the Salk Institute and a Howard Hughes Medical Institute Early Career Scientist. “The inhibitor will probably find the greatest utility in combination with targeted therapies.”
“The key to success for this project came when we combined Reuben's deep understanding of the fundamental biology of autophagy with our chemical expertise,” explained the paper's other senior author, Nicholas D.P. Cosford, Ph.D., a professor at SBP. “This allowed us to find a drug that targeted ULK1 not just in a test tube but also in tumor cells. Another challenge was finding molecules that selectively targeted the ULK1 enzyme without affecting healthy cells. Our work provides the basis for a novel drug that will treat resistant cancer by cutting off a main tumor cell survival process.”
SBI-0206965 successfully killed a number of cancer cell types including human and mouse lung cancer cells and human brain cancer cells, some of which were previously shown to be particularly reliant on cellular recycling. The group is now testing the drug in mouse models of cancer. “An important next step will be testing this drug in other types of cancer and with other therapeutic combinations,” added Dr. Shaw.
In the paper, the authors noted that since many tumors become addicted to autophagy for survival, inhibition of autophagy stands out as a potential broadly applicable cancer therapy. Drugging the autophagy pathway to combat cancer has been tried before, but the only drugs that currently block cell recycling work by targeting the cell organelle known as the lysosome, which functions at the final stage of autophagy. Although these lysosomal therapies are being tested in early-stage clinical trials, they inhibit other lysosomal functions beyond autophagy, and therefore may have additional side effects.
Such side effects could be avoided if autophagy were to be disrupted in its early stages. An attractive early-stage target, the authors knew, was ULK1/Atg1, the only serine/threonine kinase in the core autophagy pathway. To find an effective inhibitor of ULK1, the Salk and SBP scientists screened hundreds of potential molecules before they finally zeroed in on SBI-0206965, which proved to be effective not only in the test tube, but in living cells.