![Researchers at UC San Diego School of Medicine have identified pathways that regulate pancreatic ß cell (pictured in green) growth. These cells help maintain normal blood glucose levels by producing the hormone insulin. [UCSD Health]](https://genengnews.com/wp-content/uploads/2018/08/May3_2017_UCSDHealth_PancreaticBetaCell1051841718-1.jpg)
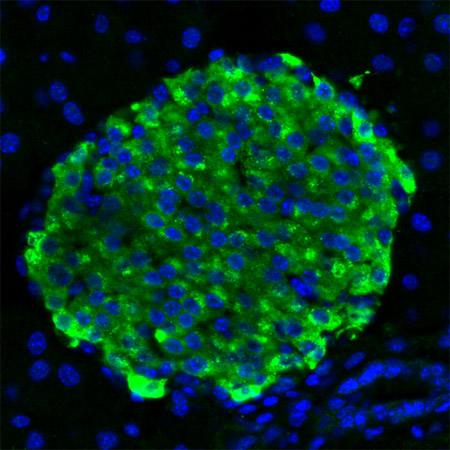
Researchers at UC San Diego School of Medicine have identified pathways that regulate pancreatic ß cell (pictured in green) growth. These cells help maintain normal blood glucose levels by producing the hormone insulin. [UCSD Health]
Scientists at the University of California San Diego School of Medicine used single-cell RNA sequencing to map out pathways that regulate β cell growth that could be exploited to trick them to regenerate.
Pancreatic β cells help maintain normal blood glucose levels by producing insulin, the master regulator of energy (glucose). Impairment and the loss of β cells interrupts insulin production, leading to types 1 and 2 diabetes. The team's study (“Pseudotemporal Ordering of Single Cells Reveals Metabolic Control of Postnatal β Cell Proliferation”) is published in Cell Metabolism.
“If we can find a drug that makes β cells grow, it could improve blood sugar levels in people with diabetes,” said Maike Sander, M.D., professor in the Department of Pediatrics and Cellular and Molecular Medicine at UC San Diego School of Medicine. “These people often have residual β cells, but not enough to maintain normal blood glucose levels.”
The body generates β cells in utero and they continue to regenerate after birth. But as people age, cell regeneration diminishes. The predominant way to grow new β cells is through cell division; but β cells capable of dividing are rare, compromising less than 1% of all β cells. Scientists have been investigating molecular pathways that govern β cell growth in hopes of finding new therapies that would help people regain blood glucose control after the onset of diabetes.
In their work, Dr. Sander's team identified the pathways that are active when β cells divide, providing insight into possible drug targets. The investigators were able to profile molecular features and metabolic activity of individual β cells to determine how dividing β cells differ from nondividing cells.
“No one has been able to do this analysis because the 1% or less of β cells that are dividing are masked by the 99% percent of β cells that are not dividing,” said Dr. Sander. “This in-depth characterization of individual β cells in different proliferative states was enabled by newer technology. It provides a better picture of what sends β cells into cell division and clues we can use to try to develop drugs to stimulate certain pathways.”
Whether stimulating β cells to grow will result in therapeutic interventions for diabetes is still to be seen, but this new information opens the door to find out, she added.