May 15, 2015 (Vol. 35, No. 10)
In the efforts to develop a system of individualized precision medical options, the integration of metabolomic pathways becomes important. Two methods are commonly used in metabolic profiling.
The first, nuclear magnetic resonance (NMR) spectroscopy, discriminates between metabolites’ proton resonance spectra; the second, mass spectrometry (MS), separates metabolites qualitatively based on molecular and chemical architecture. Analyses account for characteristic alterations in physiological states.
Metabolomic analyses often focus on mechanisms or biomarkers that can better classify one group of individuals from another set of individuals, says Scott Tebbutt Ph.D., CSO at the PROOF (PRevention Of Organ Failure) Centre of Excellence, and associate professor at the University of British Columbia.
“We end up looking at new statistical methods to integrate across different datasets,” explains Dr. Tebbutt. “It is often a complex task to integrate between modalities.”
Correlation Analyses
Dr. Tebbutt compares metabolomic datasets, typically with hundreds of molecules, to RNA microarrays and RNA-Seq, which have literally thousands of data points. Not a statistician himself, Dr. Tebbutt collaborates with Kim-Anh Lê Cao, Ph.D., a computational biologist at the University of Queensland Diamantina Institute, and other biostatistics experts.
“We use several models,” Dr. Tebbutt points out. “One such model, Sparse Generalize Canonical Correlation Discriminant Analysis, is being developed by my student, Amrit Singh, in concert with our collaborators.” This type of analysis uses a component-based approach to study relationships between several sets of variables.
In a recent study examining early and dual asthmatic responses, Dr. Tebbutt focused not just on the metabolites but on RNA, protein, and cells as well, to provide an integrated picture between single genes and single metabolites. “You perform constrained pairwise tests between genes and metabolites across all of your discovery space; sampling all the molecules you’ve actually measured,” says Dr. Tebbutt, and then from this data a correlation analysis pairs the genes, RNA, and metabolites. “You can derive these little networks, these spider webs, by tuning how your thresholds are set.”
Dr. Tebbutt was able to show that there were more networks established in the dual asthmatic responders than in the early responders. His analysis, which was presented in a 2013 PLOS ONE article, highlighted several genes including ALOX15, which codes for an enzyme that seems to interact with prostaglandin.
ALOX15 had been implicated in prostaglandin regulation in asthma previously. “We are not showing anything original in a sense,” notes Dr. Tebbutt. “We found it by basically integrating a couple datasets,” whereas others generated their data from dozens of experiments taking many years.
Dr. Tebbutt’s research is being funded by AllerGen NCE, a national research network established by Industry Canada through the Networks of Centres of Excellence program. AllerGen, which focuses on “allergy, genes, and environment,” hopes to determine whether the correlational pathways and networks studied by Dr. Tebbutt hold up in predicting particular asthmatic responses.
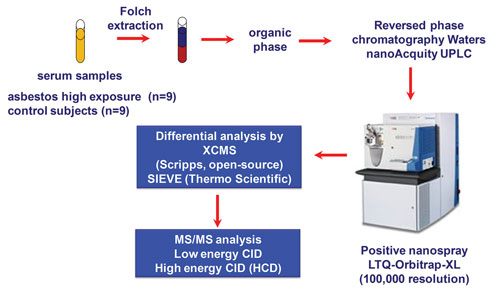
Serum Biomarkers
The focus of a significant amount of metabolomics research is the discovery of biomarkers, often used as companion diagnostics for disease therapies. Biomarker discovery researchers often use plasma, serum, or other biological products for specimen collection. Each product comes with its own set of concerns.
“We tend to use serum,” says Ian Blair Ph.D., director for the Center of Cancer Pharmacology at the Perelman School of Medicine, University of Pennsylvania.
“We have done some plasma metabolomics. The problem is there are often different anticoagulants with different samples, and all plasma samples tend to coagulate anyway, even when they are stored at −80°C, so with serum the coagulation has already taken place.” However, in general, specimen type is dependent on the analyte to be examined.
Dr. Blair studies Friedreich’s ataxia, a disease caused by a mutation in the gene frataxin or by a triplet GAA expansion in intron 1 of the gene. “You don’t need a biomarker for Friedreich’s ataxia,” notes Dr. Blair, since the mutation or triplet repeats can be picked up with a genetic screen, “but what we do need is a biomarker to show that the treatment is being successful.”
To this end, Dr. Blair and his team developed a cellular metabolism assay to look at the metabolite aconitase. “[Such an assay] is pretty tricky to do in a human,” he remarks. “We chose to use platelets and added labeled glucose to the platelets and saw how it was metabolized through the Krebs cycle.”
By using patient-specific platelets, Dr. Blair’s team was able to track 13C-labeled glucose incorporation into acetyl-CoA and succinyl CoA. A proof-of-principle study was conducted and published in Bioanalysis in 2013.
The researchers are now working with a drug company to examine the role drugs can play on correcting this metabolic dysfunction in Friedreich’s ataxia patients. “It can be overwhelming,” observes Dr. Blair. “In some experiments, we generate over 200 million chromatograms that need to be interpreted.”
Urine Biomarkers
Urine is a favored specimen type for metabolomics due to its sterile nature, relative freedom from interfering substances, and obtainability.
Jayoung Kim, Ph.D., associate professor and research scientist at Cedars-Sinai Medical Center and UCLA, studies urine metabolomics and believes that metabolomics is one of the more manageable “omics” technologies. It should, she suggests, become part of an integrative biology approach without too much difficulty. And it has relatively low instrument and method costs.
Dr. Kim and others employ teams of highly trained bioinformaticians to mine the data and compile the results. “It not really simple,” she warns, “For example, genomics and proteomics and epigenomics and metabolomics are all performed on different platforms.
“We can, however, get the signature from all of those and merge them into one single signature. We believe this approach is really important.”
Although metabolomic datasets are rather weak compared to proteomic and genomic datasets, Dr. Kim has faith in the metabolomic approach: “Within a few years, we will have a big database that we can annotate with all spectra that we could identify from past research.”
Dr. Kim, a translational scientist and a specialist in benign urology and cancer biology by training, is interested in bladder cancer and disorders of the urinary system such as interstitial cystitis. For example, Dr. Kim took part in an international collaboration that examined urine specimens and generated metabolomic profiles that were deemed to be specific to bladder cancer, especially the more aggressive bladder cancers.
In addition, Dr. Kim has used urine-based biomarker analysis to validate spectrum specific for interstitial cystitis via mass spectrometry. “Metabolomics using urine samples is very attractive to the urologist for diagnostic purposes and to monitor drug responses,” she comments.
Although urine can be collected noninvasively and is usually easily obtainable, it presents a few caveats. “As you can imagine,” cautions Dr. Kim, “diet, exercise, and environmental exposure can affect the urine metabolome.”
In addition, even though Dr. Kim and her collaborators were able to collect roughly 140 specific spectrums from the interstitial cystitis study they were unable to annotate what those spectrums meant.
According to Dr. Kim, the problem was the lack of a database: “People in this field are really trying to construct a big database for metabolic research.” Some of these findings are described in a 2015 paper in the Journal of Proteome Research.
Cancer Metabolomics
Besides an integrative approach to examining biological outcomes, via the development of urinary and serum biomarkers, many groups are interested in determining the roles of metabolites in driving tumorigenesis. Patrick Pollard, Ph.D., cancer biology and metabolism group leader at the University of Gothenburg, Sweden, has published a 2013 review on the subject for the Journal of Clinical Investigation.
“Three of the main killers in the world are diabetes, obesity, and cancer—and they all have metabolic components in them,” Dr. Pollard emphasizes. “Cancers,” he adds, “can evolve genetically and metabolically,” and he suggests that while enzymes may be mutated to become potentially oncogenic, “there is no proof that they directly cause cancer.”
Dr. Pollard points to several tumors harboring mutations in genes encoding metabolic enzymes. For example, tumors with mutations in isocitrate dehydrogenase produce 2-hydroxyglutarate, and tumors with mutations in the Krebs cycle enzymes fumarate hydratase (FH) and succinate dehydrogenase accumulate fumarate and succinate, respectively.
“We call them oncometabolites,” says Dr. Pollard, “because they are metabolites that we think might be oncogenic in high enough concentrations, but the exact contribution of these metabolic changes to tumorigenesis is yet to be determined.” His fundamental view is that genetic instability and not metabolic variability underlies cancer.
“My interest really comes from studying disease, specifically, hereditary leiomyomatosis and renal cell cancer (HLRCC) caused by inherited FH mutations.” HLRCC tumors accumulate fumarate, which activates oncogenic signaling cascades including the hypoxia and antioxidant response pathways.
FH mutant tumors exhibit high levels of hypoxia-response proteins and hypermethylation (resulting from epigenetic reprogramming). Current studies are focused on pathway targeted metabolomic analyses of renal cancers (including HLRCC tumors) and identification of metabolic biomarkers that may help stratify HLRCC and influence medical intervention.
Funding for Metabolomics
Mukesh Verma, Ph.D., chief of the epidemiology and genomics research programs methods and technologies branch at the National Cancer Institute (NCI), has also examined the role of metabolomics in cancer research and epidemiology, primarily by keeping track of funding at the federal level. “We follow spending by the NIH and the NCI,” says Dr. Verma.
The numbers suggest that metabolomics research is increasing. For example, grant-wining research projects often cite metabolomic aims—“at least one or two aims out of five,” notes Dr. Verma. An increase in metabolomics interest from small businesses is occurring as well.
“Most of the time,” Dr. Verma confides, “we are getting applications from businesses that are focused on disease diagnosis, especially cancer.” For example, a substantial increase in metabolomics funding has been seen in the field of microbiome research. Five or six bacteria have been associated with pancreatic cancer from the oral microbiome. According to Dr. Verma, this type of metabolomics research will help us in identifying pancreatic cancer, whereas previously this data could only be obtained from ribosomal RNA analysis.
In the next few years, the NCI will be asking investigators to include metabolomics along with genomics, microRNA, and microbiome data in patient-related electronic records. “[This data], states Dr. Verma, “might help us in diagnostics or detection after cancer recurrence or response to therapy.”
Ian Clift Ph.D. is a Scientific Communications Consultant, Biomedical Associates and Clinical Assistant Professor, Indiana University







